Upper age limits are used as a guide for IVF treatment on the basis of success rates. At Cairo Fertility Clinic we treat women up to the age of 45. It should be born in mind, however, that success rates with IVF treatment reduce dramatically after the female reaches 40.
IVF success rate is influenced by various factors, including the woman’s age, the cause and duration of infertility and whether the woman has been pregnant before. A good general rule is that a couple embarking upon IVF/ICSI has a 1 in 3 chance of having a live birth with each attempt. The particular circumstances that affect your individual chance will be discussed with you, and our most up to date results will be provided to you.
Steps of IVF
1. Preliminary tests:
Including a detailed semen analysis, blood tests for hormone levels such as FSH and LH, screening for viruses such as HIV, Hepatitis B and C, as well as Rubella and swabs from the cervix and vagina for bacteria and chlamydia.
2. Pituitary Suppression:
In a natural menstrual cycle, hormones from the pituitary gland (LH & FSH) cause the growth of an egg within a fluid-filled space (follicle) in the ovary. Although several follicles start to grow each month, in a natural cycle only one will become mature enough to release its egg. Release of the egg (ovulation) is triggered by a sudden surge of the hormone LH at mid-cycle. In contrast, during an IVF cycle it is desirable for several eggs to mature at once. To prevent a premature LH surge from triggering early release of these eggs, a GnRH agonist is used to temporarily turn off your own LH & FSH secretion. It is given by nasal spray or by injection.
3. Ovarian Stimulation:
After pre-treatment with a GnRH agonist, we add daily injections of LH & FSH or FSH (known as Menogon, Gonal-F, Menopur, or Puregon). The injections continue for about 10 -14 days and will stimulate the growth of several follicles. The response of the ovaries is monitored by blood tests and transvaginal ultrasounds. Most women learn to give their own injections to reduce the number of clinic visits.
4. Egg Retrieval:
Once the blood tests and ultrasounds indicate a reasonable size and number of follicles, an injection of hCG is given, causing final maturation and loosening of the egg from the wall of the follicle. The egg retrieval occurs 34 – 36 hours after hCG injection. The egg retrieval is performed by an ultrasound guided needle puncture through the top of the vagina under light general anesthetic. The fluid is drained from each follicle and examined under a microscope for the egg. Your partner is encouraged to be with you during this procedure.
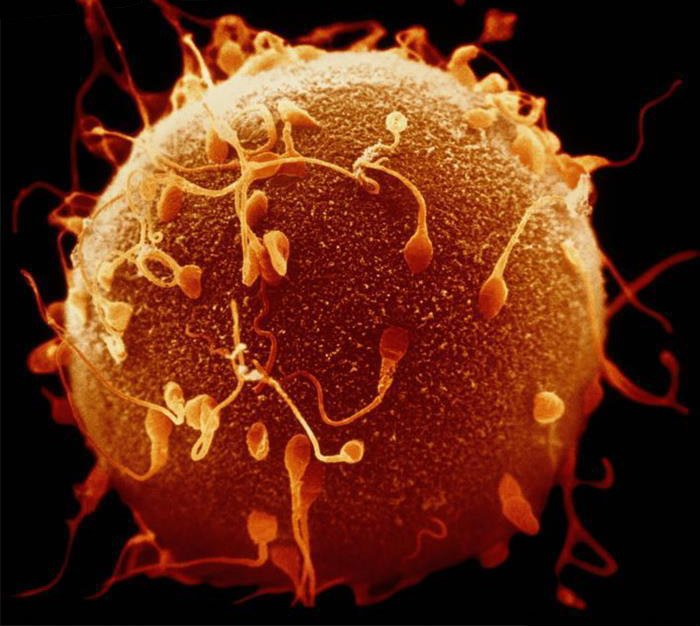
5. Fertilization:
The sperm sample is washed and concentrated, then added to the eggs a few hours after retrieval. The eggs are examined the next day for signs of fertilization. We expect about 70 – 80% of the eggs to fertilize if the sperm sample looks normal. The fertilized eggs are kept in the incubator for an additional 48 hours. Not every follicle will contain an egg, not every egg will fertilize, and not every egg that fertilizes will go on to form a good quality embryo.
6. Embryo Transfer:
Three or five days following egg retrieval, the fertilized eggs (embryos) are transferred to the uterus using a fine plastic transfer catheter. The exact number transferred depends on the woman’s age and embryo quality. This procedure takes only a few minutes and is usually not uncomfortable. Some couples will have extra embryos that are suitable for freezing. The best quality embryo(s) (those most likely to result in pregnancy) are usually transferred in the treatment cycle. To be selected for freezing, embryos must not show any signs of fragmentation (cell breakdown) or abnormal development. Obviously, not all embryos will meet these criteria.
Natural cycle IVF
Consists of IVF carried out as a part of a natural cycle. No drugs are used to stimulate the ovary to produce multiple eggs and the treatment relies on the spontaneous growth of one follicle. Hence, the drawbacks are the possibility of spontaneous ovulation occurring prior to egg retrieval, that the single egg cannot be retrieved, that the egg is not of sufficient quality to be used, or that the egg fails to fertilize in the laboratory (and that therefore no embryo transfer takes place). For these reasons the success rate of natural cycle IVF (about 7% per cycle, according to published data) is significantly lower than for stimulated cycles. Natural cycle IVF/ICSI is sometimes used in circumstances where the use of drugs for ovarian stimulation is not appropriate, where ovarian stimulation confers no benefit, or where the patient chooses not to have stimulation.
Hormonal Support after the replacement of the embryo(s)
The time after the embryos are replaced is known as the Luteal Phase. Because of the use of GnRH-analogue to suppress hormones prior to the IVF cycle beginning, the level of progesterone after embryo replacement may be reduced. For this reason it is advised that progesterone is given to help support the implantation of the embryos. Luteal Phase hormonal Support is started on the evening of the egg collection regardless of day of embryo transfer. This is given in the form of a natural progesterone called Cyclogest administered as pessaries placed rectally or vaginally (400 mg twice daily), or Gestone 100mg I.M. daily injection.
Frozen Embryos
Embryos may be frozen at any stage but only good quality embryos are classed as suitable for freezing. The embryologist will discuss with you the quality of the embryos and whether the spare embryos are of good enough quality to freeze. Around two thirds of embryos survive the freeze/thaw process. Frozen embryo replacement can be carried out in a cycle supported by HRT or in a “natural” cycle.
Pregnancy
A blood test to check for a pregnancy is carried out 14 days after embryo transfer. If the pregnancy test is positive luteal phase support is continued and an ultrasound scan will be arranged for three weeks later. This will hopefully give visual confirmation of how the pregnancy is progressing. If the scan shows an on-going pregnancy patients are scanned again 2 weeks later.
If the pregnancy test is negative, we will discuss the circumstances of the treatment and why it may have been unsuccessful. We will write to you detailing the treatment and your future options or you can make a review appointment to attend the clinic. If this has been your first treatment and spare embryos have been placed in storage, we will be able to plan with you the replacement of the frozen embryos after 2-3 months gap.
POSSIBLE RISKS ASSOCIATED WITH IVF
There are some potential risks & side effects associated with IVF procedures including:
- An exaggeration of usual menstrual cycle symptoms (e.g. bloating, breast tenderness, mood swings) because the ovaries have been stimulated to produce more than one follicle.
- In about 1% of cases, ovarian hyperstimulation syndrome (OHSS) develops. The ovaries become much enlarged and extra fluid accumulates in the abdomen. This complication requires rest, close monitoring, intravenous fluids or even drainage of the abdominal fluid. In rare cases, if we feel you are at very high risk for developing OHSS, the embryos may be frozen rather than being replaced.
- If more than one embryo is transferred into the uterus, a multiple pregnancy may occur. Multiple pregnancies carry a higher risk of preterm delivery and other associated problems. Twins can occur in 20 – 40% of cases and triplets in 1- 5%. In the latter case, a selective reduction procedure can be made available to reduce a higher multiple pregnancy down to twins, if a couple wishes.
- Fertility drugs have not been proven to increase the risk of breast, ovarian or uterine cancer; reassuring data is now available from several large follow-up studies. However, women who have never been pregnant have a higher risk of breast or ovarian cancer. Past or future use of the birth control pill will lower your risk of ovarian cancer. A yearly physical exam is important for the prevention and early detection of all diseases.
OPTIMIZING YOUR CHANCES
- Women who are underweight or markedly overweight may have difficulties during the treatment cycle or a resulting pregnancy. As medication doses and responses tend to be weight related, overweight women may require much higher dosages of medication and may have difficulty absorbing it. As well, such women have an increased risk of pregnancy loss. If you are markedly underweight or overweight, we will calculate your body mass index (BMI) and may ask you to delay treatment until your weight is in a safer range.
- If you smoke, you should attempt to quit, or at least minimize the number of cigarettes smoked each day. Women who smoke have a lower chance of becoming pregnant and a higher rate of miscarriage.
- We recommend a multivitamin supplement containing folic acid (0.4 to 1.0 mg daily) for all women who are trying to become pregnant. This B vitamin reduces the risk of some serious defects of the central nervous system in the fetus. It should be started a few weeks before the treatment begins and taken until the 10th week of pregnancy.