ICSI is most commonly recommended for:
- Couples who have failed to achieve fertilization or had very poor fertilization following standard IVF treatment.
- Men with abnormal sperm parameters (e.g. low count, poor motility, high percentage of abnormal forms and high levels of antisperm antibodies in the semen) to allow a reasonable chance of success with standard IVF.
- Azoospermic (complete absence of sperm in the ejaculate) men who have their sperm surgically retrieved. This could be due to failed vasectomy reversals or congenital absence of both vas deferenses and non-obstructive azoospermia.
- When frozen sperm is limited in number and quality.
The patient and husband’s roles in the ICSI process are the same as with a basic IVF procedure.
Ovulation induction medications are taken by the female to produce numerous eggs during one cycle and the eggs are then retrieved.
The husband will provide a semen sample by masturbation from which the healthiest sperm will be extracted. If no sperm are available naturally, a sperm retrieval procedure such as testicular biopsy, testicular sperm extraction (TESA) or percutaneous sperm aspirations (PESA) around the time of egg retrieval is scheduled.
Once the eggs and sperm have been collected, the embryologist will inject one sperm into the center of each egg.
If fertilization occurs, the healthiest embryos will be transferred into the wife’s uterine cavity.
Luteal phase support is recommended as with IVF treatment.
A blood test will be performed approximately two weeks later to determine if the patient is pregnant.
ICSI – The Process
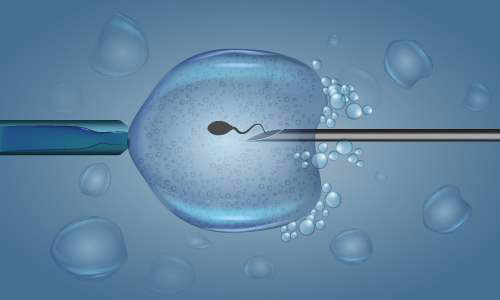
After the eggs are retrieved in an IVF cycle, they are separated from the follicular fluid, placed in a Petri dish, and examined under a microscope. The embryologist uses a micromanipulator to hold the egg in place and orient it correctly.
In the ICSI procedure, a small hole is made in the zona pellucida (egg membrane) using microscopic tools and the sperm is inserted directly into the egg. Puncturing the egg in this controlled manner does not cause damage. After insertion of the sperm (intracytoplasmic sperm injection), the embryos are placed in incubators until ready for transfer.
ICSI requires that sperm be obtained from the ejaculate if the male has sufficient quantity and quality of sperm. When adequate sperm are not available, PESA or TESA can be utilized in conjunction with intracytoplasmic sperm injection.
ICSI combined with PESA (percutaneous epididymal sperm aspiration) is a noninvasive method of sperm recovery. It requires that a small needle be placed into the epididymis, using local anesthesia, to withdraw the sperm. The epididymis normally serves as a reservoir for sperm. This technique would also be applicable for patients with congenital absence of the vas deferens, previous infection with resultant occlusion of the epididymis, and ejaculatory dysfunction due to multiple sclerosis or diabetes.
ICSI/ TESE (testicular sperm aspiration) is useful for men who have non-obstructive azoospermia caused from maturation arrest disorders and for patients in whom sperm could not be obtained through the PESA procedure. Using TESA, sperm are obtained by biopsy of the testicle. It is possible to obtain sperm using TESA even when there are none seen in the ejaculate.
The process of ICSI
- Suction applied by a glass holding pipette keeps the egg from moving during the injection. A single sperm is picked up in a tiny microneedle.
- The needle has a sharp tip and can be gently pushed through the shell of the egg and into the cytoplasm
- The sperm is deposited deep inside the egg and the empty needle is withdrawn.