Diagnosis of polycystic ovaries or syndrome
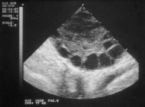
- Polycystic ovaries can only be diagnosed by ultrasound scan, the ovaries are most clearly seen by vaginal ultrasound. The diagnosis is by US finding of >/= 12 follicles 5 – 9 mm and / or a volume of > 10 mls. in the affected ovary.
- Blood tests can help to diagnose polycystic ovarian syndrome:
- LH (usually high) in relation to FSH
- Testosterone and other androgens (usually raised)
Polycystic ovaries in a woman who is not wishing to conceive and who has no symptoms related to them does not require treatment.
There are three situations where polycystic ovaries or polycystic ovarian syndrome may require treatment:
- Absent or irregular ovulation leading to difficulties in conceiving.
- Increased unwanted bodily or facial hair.
- Irregular or infrequent periods
Disorders of ovulation in a woman with polycystic ovaries can be treated by:
- Drug treatment to “induce” ovulation The most commonly used drug in this situation is clomiphene. In cases where clomiphene does not work, gonadotrophins (FSH) are needed and these are given as injections. Both these drugs require monitoring to ensure that they are producing the desired response and because of the risk of multiple pregnancy and hyperstimulation syndrome.
- Surgical treatment to the ovaries This is reserved for cases where ovulation cannot be triggered with clomiphene and gonadotrophin (injection) therapy. The technique involves using electrical energy (diathermy) or laser beams to “drill” holes in the tiny cysts that surround the ovary.
- If this strategy proves ineffective, then pursuing in vitro fertilization (IVF) is the next treatment option.
PCOS patients are advised to control their weight. This is particularly so in those women who have a raised body mass index (BMI). The best measure of fat content is the Body Mass Index (BMI). The ideal BMI is between 18 and 25. BMI is calculated in the following way: Weight in kg, divided by your height in metres squared.